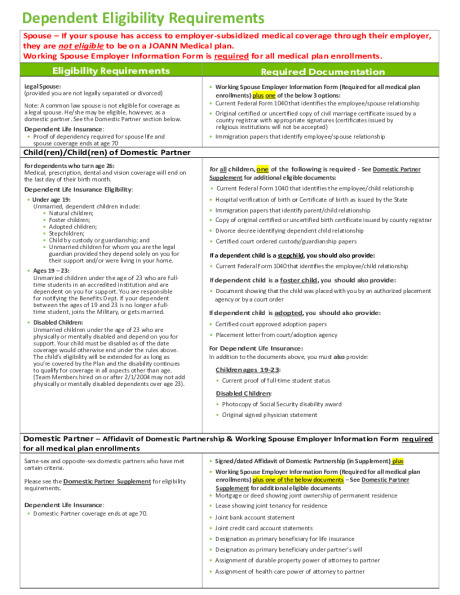
Eligible Dependents
You may also enroll your eligible dependents in many of the same plans you choose for yourself. Proof of dependent status will be required to enroll. Eligible dependents include:
- Your legal spouse or registered domestic partner
- Your natural, adopted, stepchild, or child for whom you have legal guardianship, up to age 26
- Your disabled child over the age of 26 for whom you have legal guardianship
For complete spouse and dependent children eligibility requirements, please refer to each carrier’s Certificate of Coverage.
Open Enrollment
Open Enrollment is typically scheduled for two weeks in late November or early December each year.
This is your once-a-year opportunity to pick your plans or make changes to your existing coverage. The choices you make during Open Enrollment will become effective on February 1st of the benefits plan year and will remain in effect through January 31st of that plan year.
When you enroll you can:
- Change your current coverage, if needed
- Enroll in benefits for the first time, if newly hired or newly eligible for benefits
- Update your dependent information
- Update your beneficiary information
New Employees
Team Members are eligible for benefits (full time and part time) and most coverages will begin on the first day of the month following their event date (hire date or job change date).
If you do not elect benefits during your initial enrollment period, you will not be able to make changes until the following annual open enrollment period, unless you experience a qualified life event as described below.
Qualified Life Event
Because contributions to Medical, Dental, Vision, Health Savings and Flexible Spending Accounts are made on a before tax basis, Federal laws require your elections to remain in effect for the entire plan year.
Certain life events provide you a 31-day window to elect benefits or change your covered dependents.
What is a Qualified Life Event? If you experience any of the scenarios below, you may be eligible to update your benefit elections mid-year:
- Marriage, divorce, or legal separation
- Birth or adoption of a child
- Commencement or termination of adoption proceedings
- Change in child’s dependent status
- Death of a dependent
- Loss or gain of other health coverage for you and/or dependents
- Change in employment status
- Change in residence due to an employment transfer for you or your spouse
- Change in Medicaid/Medicare eligibility for you or a dependent
- Receipt of a Qualified Medical Child Support Order
- Court Order
Remember, dependent verification will be required.
If you have questions about your eligibility or enrollment process, check with your plan administrator.